Marc Darrow, MD.
We are often asked if certain injections will accelerate ACL repair after ACL reconstruction. The answer is, it depends on the patient and the surgery. In this article we will look at research surrounding PRP, stem cells and hyaluronic acid.
A September 2024 study (1) writes: “Emerging trends and future directions in ACL reconstruction are centered on advancements in biological augmentation, innovations in surgical techniques, and the need for comprehensive long-term outcome studies. Biological augmentation methods, such as platelet-rich plasma and stem cells, are increasingly recognized as promising options for enhancing ACL repair and reconstruction. These biological agents aim to create a more conducive healing environment for the graft, which could lead to improved clinical outcomes.” 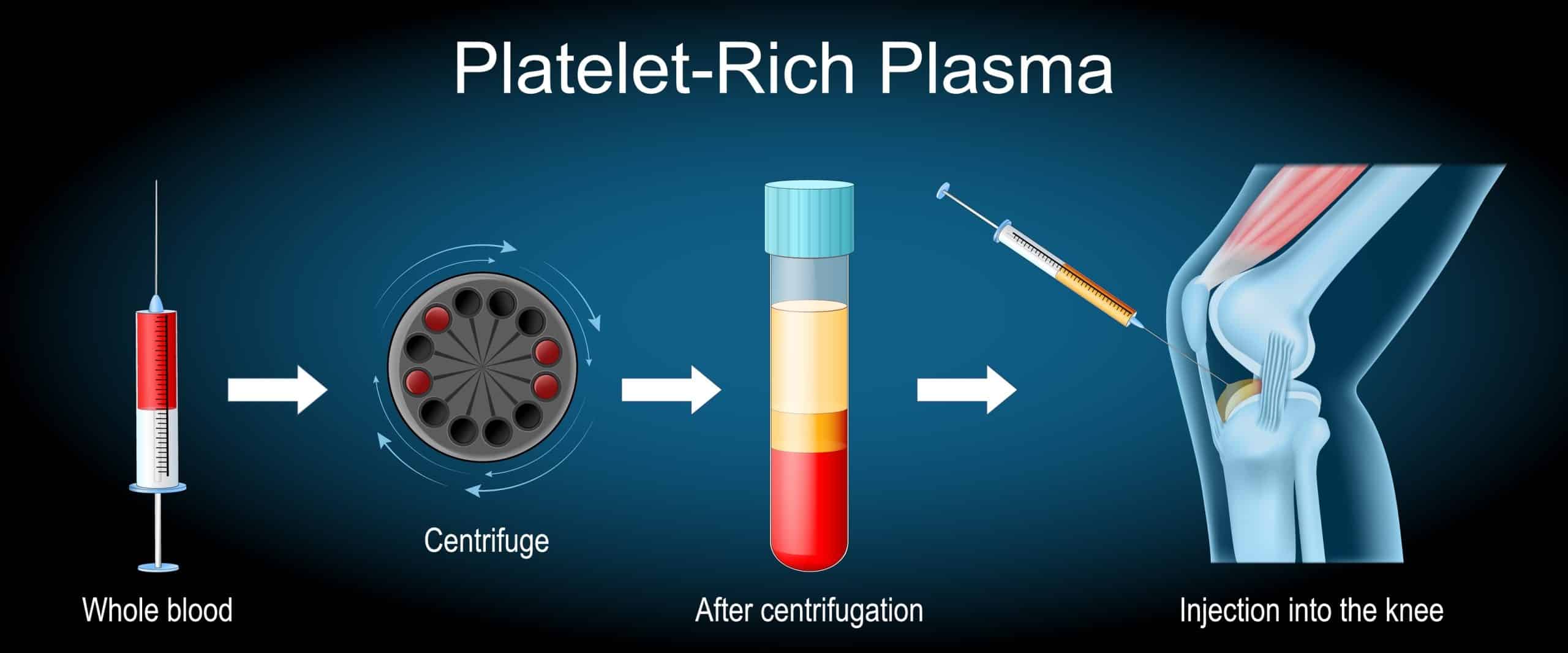
Injections post-ACL Reconstruction. What’s the evidence?
Researchers did not find any clinical benefit of intraarticular hyaluronic acid injection following ACLR surgery
A March 2022 paper (2) examined the problems of pain, swelling and joint stiffness following arthroscopic ACL reconstruction (ACLR) surgery. The researchers examined post published medical research and identified four studies that would best answer their question on the effectiveness of intraarticular hyaluronic acid injection following ACL reconstruction (ACLR).
- There were 182 patients in the intraarticular hyaluronic acid injection group and 121 patients in the control group. In comparison analysis the researchers found: “Although the individual study demonstrated a short-term positive response regarding pain control and swelling reduction, the pooled analysis did not find any clinical benefit of intraarticular hyaluronic acid injection following ACLR surgery.”
A January 2023 study (3) looked at the data of 951 patients over 12 previously published studies and found in patients who had hyaluronic acid injections following arthroscopic knee surgery, including ACL reconstruction, “the available evidence does not support its efficacy in pain relief and functional recovery. Therefore, the application of intraarticular hyaluronic acid injection after arthroscopic knee surgery is not recommended.”
PRP Injections
Platelet Rich Plasma Therapy or sometimes referred to as PRP is a regenerative / biologic therapy that uses the healing factors of your blood to rebuild and repair damaged tissue. Doctors have been using this treatment for many years because PRP can be seen as an alterative to cortisone injection and surgical intervention.
An August 2023 study (4) suggested PRP Injections may help accelerate healing after ACL reconstruction. In this study, 80 patients who underwent ACL reconstruction were randomly assigned to receive either PRP or standard treatment. After 6 months, the group treated with PRP showed improved healing and better knee function compared with the non-PRP group. These findings suggest that PRP can help accelerate ACL healing and improve outcomes for patients. A 2022 paper did not support the use of PRP. (5) The main finding was that only a few publications demonstrated a positive effect of PRP on accelerating the maturation process of tendon graft and healing processes on bone tunnel and the harvest site of autologous graft, and the clinical outcomes could hardly be significantly improved following application of PRP.
In a January 2024 study (6), doctors administered PRP therapy within six weeks after ACL injury in patients who expressed the desire for an early return to sports through conservative care. After the treatment, patients wore a simple brace that limited deep flexion but placed no restrictions on weight bearing. Four months was the standard goal established for returning to pre-injury condition. The average patient age was 32.7 years and the average treatment was 2.8 PRP sessions.
MRI evaluations confirmed that ligament continuity was regained in all cases. All the patients returned to their pre-injury level in an average of 139.5 days, but there was one instance of re-rupture following the return to sports.
What about older patients? PRP injections or ACL Surgery?
Here we will briefly touch on the non-surgical option of PRP, especially in the older patient. PRP treatments involve collecting a small amount of your blood and spinning it in a centrifuge to separate the platelets from the red cells. The collected platelets are then injected back into knee to stimulate healing and regeneration. PRP injections do not grow a new ACL, they strengthen the other support structures within the knee to help offset ACL deficiency.
An August 2022 study (7) compared PRP injections to ACL reconstructive surgery outcomes in older patients. These are the findings: “In old patients with ACL rupture, surgery is not recommended due to the person’s low level of activity and knee osteoarthritis. Platelet-rich plasma (PRP) is a good treatment option in inflammatory cases in orthopedics.” This study was to assess and comparison of the effect of PRP and arthroscopic surgery on anterior cruciate ligament rupture.
- 100 patients were randomly divided into two groups.
- The first group of patients underwent ACL tendon repair surgery by arthroscopy and tendon graft.
- The second group were treated by PRP injection.
- Patients in both groups had significant improvements in decreased pain severity after 14 months. The surgical treatment group had lower pain and higher range of motion compared to PRP group.
For the older patient PRP presented a non-surgical option that was comparable to ACL reconstruction.
Stem Cell Therapy for ACL tears
Are stem cells an option to ACL reconstruction? Mesenchymal stem cells are injected into the area of the ACL tear. The theory is that the stem cells can deliver and help produce healing factors to repair damaged cells and stimulate tissue regeneration.
In December 2019, a study from the Mayo Clinic (8) suggested that stem cell therapy may offer a viable enhancement to post-surgical ACL reconstruction repair. They write, “As regenerative medicine continues to rapidly evolve, the use of stem cells in ligament repair and reconstruction continues to be investigated and grow. Various stem cell preparations are available in clinical practice . . .To date, there is a relative paucity of high-level evidence for the use of stem cells in ligament surgery and healing; however, early human and animal results support the reparative and immunomodulatory potential of stem cells as an evolving therapeutic meriting further investigation. . .improved outcomes spanning from higher patient-reported outcome scores to magnetic resonance imaging evidence of ligament healing in the setting of anterior cruciate ligament tears.”
The idea of improvement to surgery is expressed in many patients we see for ACL tears and knee problems who are unfortunately on their second or even third ACL reconstruction surgery recommendation. They are weighing their options knowing already what a surgery and rehabilitation will be like. For them the appeal of surgery has lost some luster.
During the surgery: PRP and bone marrow aspirate used during ACL reconstruction
A January 2024 study (9) examined the outcomes of bone marrow aspirate concentration and PRP applied during ACL reconstruction. (The study indicated the limited enhancing effect in clinical function, (ACL) graft maturation and tendon–bone interfacial healing, with only significant knee laxity improvement in the bone marrow aspirate concentration + PRP group at 24 weeks compared with the control group (no biologic augmentation).
Free phone consultation
Schedule a free phone consultation today and receive our exclusive Regenerative Medicine Stem Cell & PRP Quick Start Guide —a digital resource packed with:
- Insights into Stem Cell & PRP Therapy
- Research-backed treatments for chronic tendon injuries, joint pain, arthritis, and sports injuries
Take the first step toward a pain-free, active life today.
Call for a free phone consultation with our staff 800-300-9300
1 Gharpinde MR, Jaiswal AM, Dhanwani Y. A Comprehensive Review of Graft Choices and Surgical Techniques in Primary Anterior Cruciate Ligament Reconstruction: An Outcome Analysis. Cureus. 2024 Sep;16(9).
2 Tripathy SK, Varghese P, Behera H, Balagod R, Rao PB, Sahoo AK, Panda A. Intraarticular viscosupplementation following arthroscopic anterior cruciate ligament reconstruction: A systematic review. Journal of Clinical Orthopaedics & Trauma. 2022 May 1;28.
3Mao B, Pan Y, Zhang Z, Yu Z, Li J, Fu W. Efficacy and safety of hyaluronic acid intra‐articular injection after arthroscopic knee surgery: a systematic review and meta‐analysis. Orthopaedic Surgery. 2023 Jan;15(1):16-27.
4 Munde K, Banerjee S, Gahlot N, Elhence A, Mandal S, Yadav T. Effect of platelet-rich plasma on healing of autologous graft after anterior cruciate ligament reconstruction: a randomized control trial. Regenerative Medicine. 2023 Aug;18(8):601-10.
5 Cao Y, Wan YD. Effectiveness of Platelet‐Rich Plasma in Anterior Cruciate Ligament Reconstruction: A Systematic Review of Randomized Controlled Trials. Orthopaedic Surgery. 2022 Oct;14(10):2406-17.
6 Hada S, Hada M, Yoshida K, Kaneko H, Saita Y, Kubota M, Ishijima M. Conservative Treatment Using Platelet-Rich Plasma for Acute Anterior Cruciate Ligament Injuries in Highly Active Patients: A Retrospective Survey. Cureus. 2024 Jan;16(1).
7 Eslami S, Fattah S, Taher SA, Rezasoltani Z. Platelet-rich plasma therapy or arthroscopic surgery on repair of anterior cruciate ligament rupture. Eur J Transl Myol. 2022 Aug 1.
8 Hevesi M, LaPrade M, Saris DB, Krych AJ. Stem Cell Treatment for Ligament Repair and Reconstruction. Current Reviews in Musculoskeletal Medicine. 2019 Jan 1:1-5.
9 Lin YC, Chen YJ, Fan TY, Chou PH, Lu CC. Effect of bone marrow aspiration concentrate and platelet-rich plasma combination in anterior cruciate ligament reconstruction: a randomized, prospective, double-blinded study. Journal of Orthopaedic Surgery and Research. 2024 Jan 3;19(1):4.






