Marc Darrow, MD, JD
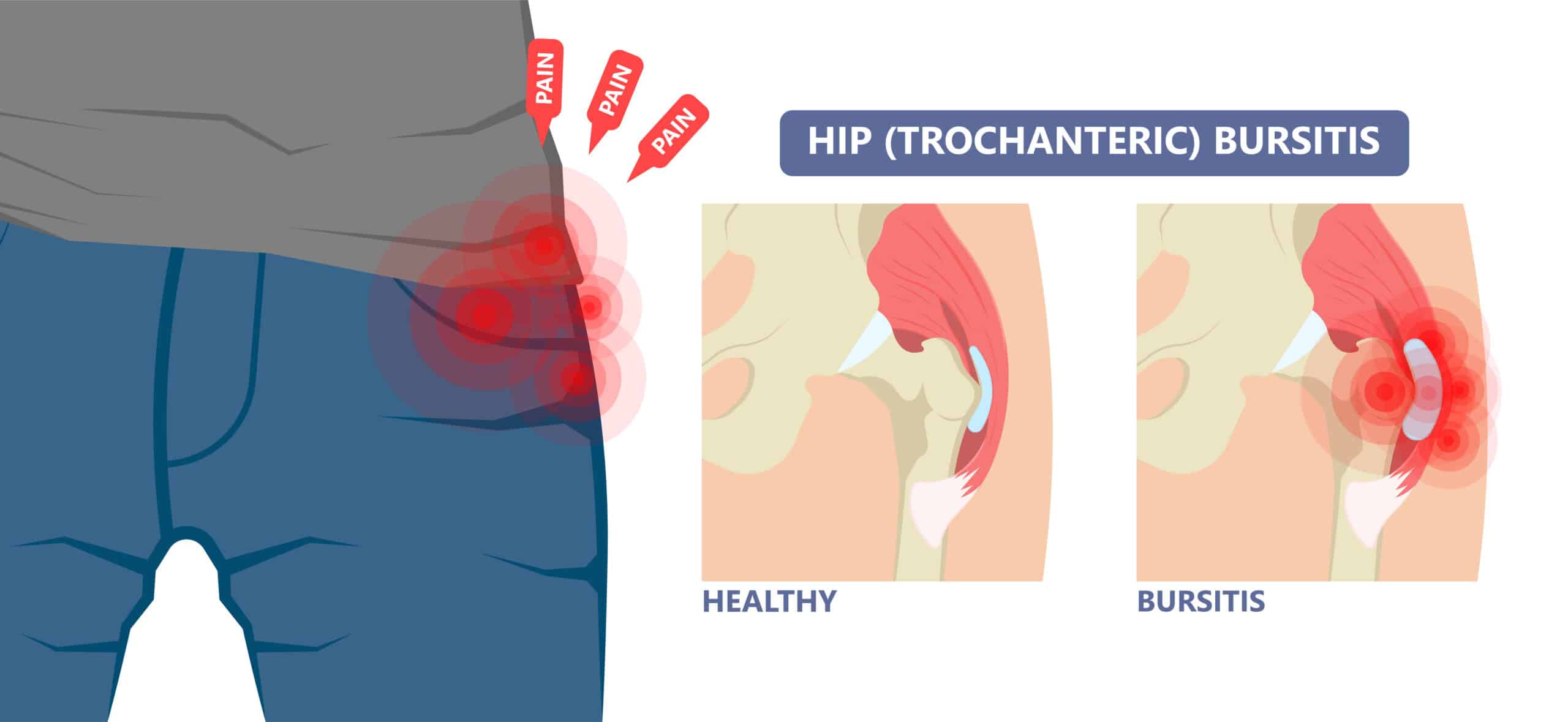
Over the years we have seen many patients with hip pain. Many of them having a “hip bursitis,” or more commonly a trochanteric bursitis or iliopsoas bursitis. Sometimes both. The iliopsoas bursitis is felt in the groin area on the inside of the hip. The trochanteric bursitis is felt on the outer part of the hip.
However, most of the patients we see may or may not have a bursitis even though they have a diagnosis of one and they are on anti-inflammatory medications. Bursitis is an inflammation of the protective, fluid filled sacs that prevent excessive friction between the functional soft tissue of the hip, i.e., the ligaments and tendons, and the bones they attach to and rub against. These bursae can become irritated from injury, excessive pressure, and overuse. More often this diagnosis is actually a problem of tendonitis or tendinosis. However, for the purpose of this article, I will focus on the problem of bursitis.
A Review of Greater trochanteric pain syndrome
traditional treatment methods
“There is no clear consensus on the optimal management approach for this condition,” according to a June 2025 study published in the journal Cureus (18). The study assessed current treatments and proposed that “targeted physiotherapy offers superior long-term outcomes compared to shock wave therapy and corticosteroid injections.” Moreover, “Although PRP has shown potential in some studies, further research is necessary before it can be recommended as part of standard treatment protocols.”
The online medical publication STATPEARLS (1) (updated February 2024) describes trochanteric bursitis management as typically including “activity modification, physical therapy, weight loss, corticosteroid injection, and nonsteroidal anti-inflammatory medications (NSAIDs). The initial approach to treat greater trochanteric pain syndrome includes a range of conservative interventions such as physiotherapy, local corticosteroid injection, platelet-rich plasma (PRP) injection, shockwave therapy (SWT), activity modification, pain-relief and anti-inflammatory medication, and weight reduction. Most cases resolve with conservative measures, with success rates of over 90%.”
These treatments may be effective for many people as attested to in the citation above, up to 90% of the time. However they will be non-effective for others. Once the cortisone injection or injections fail to provide any relief, the patient will usually start seeking other options.
Corticosteroids, platelet-rich plasma, hyaluronic acid, dry needling, structured exercise programs and extracorporeal shockwave therapy
A July 2022 study (2) compared the effectiveness of the various nonoperative treatments for greater trochanteric pain syndrome including injections of corticosteroids, platelet-rich plasma, hyaluronic acid, dry needling, structured exercise programs and extracorporeal shockwave therapy. Thirteen randomized controlled trials and 1034 patients were included. For pain scores at 1 to 3 months follow-up, both platelet-rich plasma (PRP) and shockwave therapy demonstrated significantly better pain scores compared with the no treatment control group with PRP having the highest probability of being the best treatment at both 1 to 3 months and 6 to 12 months. No proposed therapies significantly outperformed the no treatment control group for pain scores at 6 to 12 months. Structured exercise had the highest probability of being the best treatment for improvements in functional outcomes and was the only treatment that significantly improved functional outcome scores compared with the no treatment arm at 1 to 3 months. Conclusion: Current evidence suggests that PRP and shockwave therapy may provide short-term (1-3 months) pain relief, and structured exercise leads to short-term (1-3 months) improvements in functional outcomes.
Corticosteroid injections and shock wave therapy
A May 2023 study (3) compared the effectiveness of corticosteroid injections and shock wave therapy in the treatment of greater trochanteric pain syndrome. This study included 12 men, 48 women with an average age of about 51. The patients were randomly assigned to two groups, 32 patients getting shock wave therapy one session per week for a total of three weeks, the second group of 28 patients had corticosteroid injection and local anesthetic. Both groups were evaluated and the outcome results show that both corticosteroid injections injection and shock wave therapy are effective modalities and (neither) of the treatments is superior to each other.
Exercise compared to corticosteroid injection
A June 2024 study (4) explored the effectiveness of exercise versus other conservative treatments in patients with Greater Trochanteric Pain Syndrome (GTPS). In this study, 733 patient outcomes from six previously published studies were examined. In these six studies, three compared exercise to sham exercise or wait-and-see control groups, two trials compared exercise to corticosteroid injection, two trials compared exercise to shockwave therapy, and one trial compared exercise to another type of exercise.
When the outcomes were compared, the researchers wrote: “The current evidence supports a strong recommendation for exercise as first line treatment in patients clinically diagnosed with Greater Trochanteric Pain Syndrome (GTPS). Compared to corticosteroid injection, exercise is superior in increasing the likelihood that a patient experiences a meaningful global improvement.”
Shock wave therapy versus therapeutic exercise
A June 2023 paper (5) compared effectiveness of shock wave therapy versus therapeutic exercise, including the possibility of combining both therapies, in patients who did not respond to the first treatment. According to the paper the researchers were able to valid the effectiveness of both treatments (therapeutic exercise and shock wave therapy) in both single and combined modalities in patients not responding to a single treatment. . . . This combined treatment strategy allowed patients who had no benefit in terms of pain reduction after 2 months to recover promptly. However, although both treatments were effective, it was found that patients who received shock wave treatment alone had a more marked recovery from a functional point of view.
A June 2024 study (6) examined the effectiveness of shockwave therapy alone in the treatment of greater trochanteric pain syndrome. The researchers of this study reviewed the data of twelve articles (1121 subjects). They found: “Moderate-quality evidence demonstrated no statistically significant improvements in pain and function post-shockwave therapy compared to control. Low-quality evidence established clinical improvements throughout all included studies favoring shockwave therapy over control. Consequently, owing to relatively low incidence of side effects, shockwave therapy should be considered a viable option for the management of greater trochanteric pain syndrome.”
Bipolar pulsed radiofrequency and steroid injection
A December 2023 study (7) assessing ultrasound-guided bipolar pulsed radiofrequency and steroid injection targeting the trochanteric branches of the femoral nerve, presented the outcomes of treatment in nine patients with Greater trochanteric pain syndrome. Based on self-reported questionnaires, the clinicians found a favorable outcome for most patients with 8 of the 9 patients achieving a 50% reduction of pain at six month follow up.
Please see our article on PRP injections
When surgery is indicated for greater trochanteric pain syndrome?
A conscious statement from the doctors of the The 2022 International Society for Hip Preservation (15) suggested that “the indications for surgical management vary based on individual patient characteristics and surgeon-specific criteria. These findings may include imaging evidence of a Gluteus Medius tear, failed previous appropriate conservative management, a severe gait deviation, the inability to abduct hip against gravity, and tissue quality. Although 60–90% of individuals with Greater trochanteric pain syndrome will respond positively to conservative management, those with prolonged pain and dysfunction despite appropriate conservative interventions may require surgical intervention.”
In this March 2023 study (16) of 33 patients, the authors suggested “endoscopic surgery for greater trochanteric pain syndrome improved patient-reported outcomes and the procedure was associated with low risk of complications.” The authors also noted “a 71% satisfaction rate with the surgery.”
Managing glucose levels may help prevent trochanteric bursitis
A September 2023 study (17) looked at diabetes mellitus as a possible risk factor for the development of trochanteric bursitis. In this study, the research team assessed the medical data of (55,428 people without diabetes mellitus and 5182 with diabetes mellitus), of whom 5418 were diagnosed with diabetes mellitus.
The paper finds “the odds of individuals with diabetes mellitus being diagnosed with trochanteric bursitis were 55.8% higher compared to the odds of patients without diabetes mellitus. (The researchers also) found that insulin users had a lower risk of trochanteric bursitis than patients not using insulin. Females are 3.3 times more likely to have trochanteric bursitis than males.” The conclusion of this research was: “diabetes mellitus is a risk factor for developing trochanteric bursitis. Insulin had a protective effect against trochanteric bursitis, suggesting that better glycemic control might prevent this painful infliction. ”
Call for a free phone consultation with our staff 800-300-9300
References
1 Pumarejo Gomez L, Childress JM. Greater Trochanteric Pain Syndrome. [Updated February 2024]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
2 Gazendam A, Ekhtiari S, Axelrod D, Gouveia K, Gyemi L, Ayeni O, Bhandari M. Comparative Efficacy of Nonoperative Treatments for Greater Trochanteric Pain Syndrome: A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials. Clinical Journal of Sport Medicine: Official Journal of the Canadian Academy of Sport Medicine. 2021 Mar 12.
3 Yağcı HÇ, Yağcı İ, Bağcıer F. Comparison of shock wave therapy and corticosteroid injection in the treatment of greater trochanteric pain syndrome: A single-blind, randomized study. Turkish Journal of Physical Medicine & Rehabilitation (2587-1250). 2023 Jun 1;69(2).
4 Kjeldsen T, Hvidt KJ, Bohn MB, Mygind-Klavsen B, Lind M, Semciw AI, Mechlenburg I. Exercise compared to a control condition or other conservative treatment options in patients with Greater Trochanteric Pain Syndrome: a systematic review and meta-analysis of randomized controlled trials. Physiotherapy. 2024 Jan 5.
5 Notarnicola A, Ladisa I, Lanzilotta P, Bizzoca D, Covelli I, Bianchi FP, Maccagnano G, Farì G, Moretti B. Shock Waves and Therapeutic Exercise in Greater Trochanteric Pain Syndrome: A Prospective Randomized Clinical Trial with Cross-Over. Journal of Personalized Medicine. 2023 Jun 10;13(6):976.
6 Harding D, Cameron L, Monga A, Winter S. Is shockwave therapy effective in the management of greater trochanteric pain syndrome? A systematic review and meta‐analysis. Musculoskeletal Care. 2024 Jun;22(2):e1892.
7 Vieira A, Coroa MC, Carrillo-Alfonso N, Correia FD, Coroa M, Correia F. Treatment of Greater Trochanteric Pain Syndrome With Ultrasound-Guided Bipolar Pulsed Radiofrequency of the Trochanteric Branches of the Femoral Nerve: A Case Series of Nine Patients. Cureus. 2023 Dec 12;15(12).
8 Pianka MA, Serino J, DeFroda SF, Bodendorfer BM. Greater trochanteric pain syndrome: Evaluation and management of a wide spectrum of pathology. SAGE Open Medicine. 2021 Jun;9:20503121211022582.
16 Karlsson L, Quist P, Helander KN, Snaebjörnsson T, Stålman A, Lindman I, Öhlin A. Good functional outcomes after endoscopic treatment for greater trochanteric pain syndrome. Journal of Experimental Orthopaedics. 2023 Mar 15;10(1):26.
17 Kadar A, Itzikovitch R, Warschawski Y, Morgan S, Shemesh S. Diabetes Mellitus Is a Possible Risk Factor for the Development of Trochanteric Bursitis—A Large-Scale Population-Based Study. Journal of Clinical Medicine. 2023 Sep 24;12(19):6174.
18 Gill JK, Neal-Smith G, Saed A, Burgan A, Fernquest S. Management of Greater Trochanteric Pain Syndrome: A Narrative Review. Cureus. 2025 Jun 12;17(6).






