Marc Darrow, MD, JD.
People have very successful shoulder surgeries. Most go very well. But what about the few that do not? We do a lot of research in our clinic, one topic we research often is shoulder osteoarthritis. Most research articles deal with the surgical aspect and the various types of surgical techniques that can be offered the patient. There are also many new studies on the problems of shoulder replacement and fixing a failed replacement. I wrote an extensive article in 2017 on the problems of shoulder replacement complications. That article has been built on here with new 2025 research that continues to show the problems some patients face following a shoulder replacement. The research below can help inform patients that the realistic outcome some patients can expect is that when they agree to the shoulder replacement surgery, is they should be prepared for the likely outcome of the necessity for multi-surgeries.

The incidence of shoulder replacement complications
An August 2023 study (1) used computed tomography (CT) to determine the incidence of shoulder replacement complications.
- Eight hundred twelve CTs in 797 unique patients were included (438 (53.9%) females and 374 (46.1%) males; average age 67).
- There were:
- 403 total shoulder replacements,
- 317 reverse total shoulder replacements, and
- 92 hemiarthroplasties.
- Complications were present in 527/812 (64.9%) and incidences were:
-
- loosening/aseptic osteolysis 36.9%,
- periprosthetic failure 21.6%,
- periprosthetic fracture 12.3%,
- periprosthetic dislocation 6.8%,
- joint/pseudocapsule effusion 5.9%,
- prosthetic failure 4.8%,
- infection 3.8%, and
- periprosthetic collection 2.1%.
-
- In this study, the incidence of shoulder replacement complication identified on CT was 64.9% and the most commonly occurring complication was loosening/aseptic osteolysis (36.9%). Total shoulder replacement had the highest incidence of complication (75.7%).
Here is a recent study from a Swedish research team. It appears in the journal Acta orthopaedica (2) and discusses shoulder hemiarthroplasty. Shoulder hemiarthroplasty is a procedure where the ball of the shoulder is replaced with a prosthetic, while the socket (or tee) remains intact.
The two types of Shoulder hemiarthroplasty are:
- shoulder resurfacing hemiarthroplasty (a protective metal cap is placed over the ball of the humerus head)
- shoulder stemmed hemiarthroplasty (imagine a thumb tack, the metal cap is attached to a metal stem which is pushed into the humerus head)
Shoulder hemiarthroplasty comes with a high risk of need for second surgery. To quote the research: “. . . while patients receiving resurfacing hemi and stemmed hemi, reported similar shoulder functionality and quality of life, the revision rate for resurfacing hemi (12%) . . . stemmed hemi (6.7%).
The purpose of this study was to find why there was such a difference.: The results were:
- The younger patients were more likely to receive the resurfacing shoulder hemiarthroplasty and since younger people live longer, the chances of need or more revision surgery is greater. So a skewed result is achieved resurfacing shoulder hemiarthroplasty have a higher risk for revision because the patients were young enough to have multiple surgeries.
- The older you were, the more likely you would get the shoulder stemmed hemiarthroplasty because you suffered from primary osteoarthritis. Then you had a 6.7% chance of going back to surgery. Since the patients were older, as we have seen in other studies, they would be less likely to want to undergo a second or revision surgery. Older adults fearful of revision surgery also can skew results.
Does comprehensive arthroscopic management for glenohumeral osteoarthritis adversely affect outcomes after subsequent total shoulder replacement?
A June 2021 paper (3) examined if people who had a failed arthroscopic shoulder surgery would be at risk for a failed total shoulder replacement. Patients younger than 70 years who underwent primary total shoulder replacement or arthroscopic surgery first then total shoulder replacement were examined at least two years after their last surgery. There were 56 patients in total at the end of the study. Of which 19 patients had the arthroscopic surgery first then total shoulder replacement and 37 patients had the total shoulder replacement without prior arthroscopic shoulder surgery.
- There were 4 patients (7.1%) who had failure, and failure rates did not differ significantly between the arthroscopic surgery first then total shoulder replacement (5.3%) and primary total shoulder replacement only group.
- Additionally, 2 patients underwent revision arthroplasty because of trauma.
- A total of 50 patients who did not experience failure (17 arthroscopic surgery first then total shoulder replacement and 33 primary primary total shoulder replacement) completed patient surveys at almost five years after their last surgery measures with no significant difference between the arthroscopic surgery first then total shoulder replacement and primary primary primary total shoulder replacement.
- Both groups improved significantly from preoperatively to postoperatively in all survey scores.
The conclusion of this research: “Patients with severe glenohumeral osteoarthritis who failed previous arthroscopic surgery benefited similarly from total shoulder replacement compared with patients who opted directly for total shoulder replacement.”
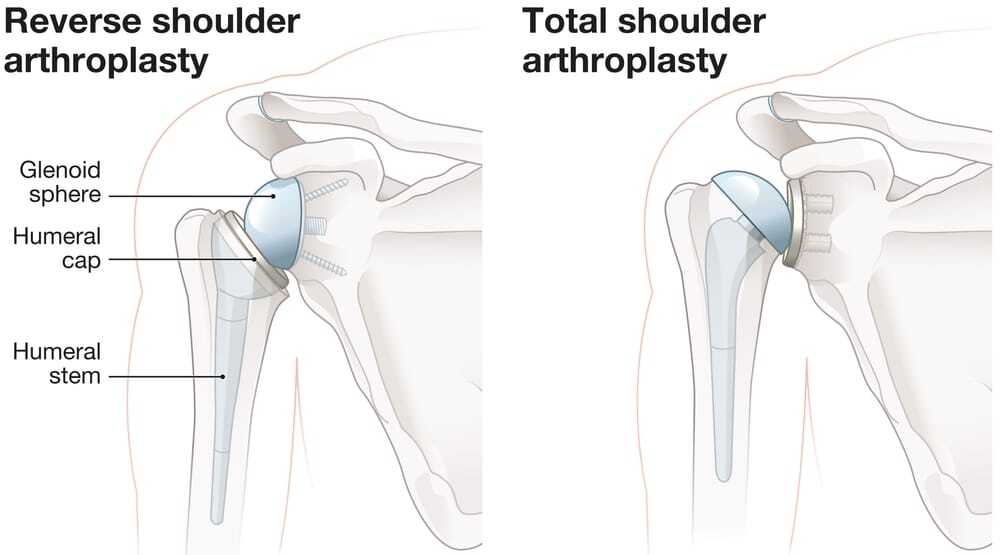
Reverse total shoulder replacement
An August 2022 paper (4) compared Reverse total shoulder arthroplasty replacement with standard total shoulder arthroplasty (replacement). These are the findings: “Reverse total shoulder arthroplasty (Reverse total shoulder arthroplasty replacement), which was originally designed mainly for irreparable rotator cuff damage, has gained popularity in recent years for the treatment of advanced shoulder osteoarthritis instead of the clinically standard total shoulder arthroplasty (replacement). However, this Reverse total shoulder arthroplasty has some nonnegligible flaws such as higher complications rate and economic cost, not mention the following problems caused by irreversible physical structural damage. Therefore, the employment of Reverse total shoulder arthroplasty needs to be carefully considered.”
In this study of 57,156 shoulder arthroplasties, “Reverse total shoulder arthroplasty patients in the rotator cuff deficiency group had significant higher transfusion rates and longer hospital stays. Reverse total shoulder arthroplasty patients without rotator cuff deficiency had a statistically significantly higher number of implant-related mechanical complications, acute upper respiratory infections and postoperative pain. Overall, Reverse total shoulder arthroplasty incurred higher costs in both groups. For osteoarthritis patients with rotator cuff deficiencies, Reverse total shoulder arthroplasty has its benefits as complication rates were comparable to total shoulder arthroplasty. For those patients without rotator cuff deficiencies, the use of Reverse total shoulder arthroplasty should be reconsidered as there were more complications with higher severity.”
A December 2023 paper (5) found: “Patients with specific risk factors and co-morbidities are predisposed to developing periprosthetic dislocation after reverse shoulder replacement. Risk factors that were found to be associated with a higher incidence of periprosthetic dislocation are gender (female), race (Caucasian), and age (young patients). Analysis revealed the history of tobacco-related disorder, obesity, morbid obesity, liver cirrhosis, and Parkinson’s disease increased the odds of developing periprosthetic dislocation following reverse shoulder replacement.”
A September 2022 paper (6) looked at patients who had a reverse total shoulder replacement to try to determine increased risk factors for shoulder instability following the surgery. The researchers examined outcomes in 194 reverse total shoulder replacements. Seven patients suffered a prosthetic dislocation signifying shoulder instability post-surgery. The dislocation occurred 60 weeks after the surgery. Five of the seven patients had a revision surgery. In these patients the researchers found being overweight or obese, worse health, or an oversized prosthetic liner would lead to greater complication risk.
A paper from December 2021 (7) examined if the severity of osteoarthritis and the development of bone spurs at the acromioclavicular joint would lead to post reverse shoulder replacement fractures of the acromial and scapular spine fractures. In this study 11 patients, who were about 70 years old, who had complications were matched to 44 patients who did not. The patients who suffered either an acromial or scapular spine fractures post-operatively had worse acromioclavicular joint osteoarthritis larger osteophyte or bone spur formation.
A long history of shoulder instability could make replacement outcomes worse
A 2022 paper (8) citing the above research says this: “We found worse outcomes for patients with previous surgery for instability independent of age, sex, and arthroplasty (resurfacing the bones or joint replacement) type. The reason cannot be deduced from this study and there is no adequate explanation in the literature. Several factors could, in theory, have an adverse effect on the outcome for these patients. A long history of instability and previous surgery may lead to eccentric glenoid wear and subsequently a technically demanding operation with risk of persisting instability, subluxation of the humeral component, or loosening of the glenoid component.”
What was the outcome of the necessity for revision shoulder replacement surgery in this study group?
An August 2021 study (9) assessed the rate of complications associated with the need to recommend patients to a revision shoulder arthroplasty.
Patients were recommended to a revision shoulder replacement surgery because of:
- component loosening 20% (601 patients of 3,041 patients in the study)
- shoulder instability 19% (577 patients of 3,041 patients),
- rotator cuff failure 17% (528 patients of 3,041 patients),
- and infection 16% (490 patients of 3,041 patients).
Many people have rotator cuff repair prior to shoulder replacement. The hope of course is that arthroscopic rotator cuff will improve rotator cuff problems and repair rotator cuff defect. In these surgeries rotator cuff healing may not occur and then the patients will develop rotator cuff disease.
Revision complications
- Intraoperative complication (complication during the revision surgery) was 8% (230 of 2,915 patients in the study)
- Postoperative complication was 22% (825 of 3,843 patients in the study), and
- Reoperation rates were 13% (584 of 3,843 patients in the study).
For various reasons some chose not to have the secondary surgery. The authors concluded: “Satisfactory improvement in patient-reported outcome measures are reported following revision shoulder arthroplasty; however, revision surgery is associated with high complication rates and better outcomes may be evident following revision to reverse shoulder replacement.”
The risk in elderly patients needing a revision shoulder replacement
An April 2023 study (10) examined the risk in elderly patients needing a revision shoulder replacement. Reverse total shoulder replacement (RTSA), initially indicated for cuff tear disease, is increasingly used for elderly patients with primary glenohumeral osteoarthritis and an intact rotator cuff. This is often done to avoid revision surgery in elderly patients for rotator cuff failure with anatomic total shoulder replacement. Despite traditionally good outcomes of total shoulder replacement. Reverse total shoulder replacement and total shoulder replacement for glenohumeral osteoarthritis with an intact rotator cuff in patients over 70 years had a similar revision risk, as well as likelihood for 90-day emergency room visits and readmissions. While revision risk was similar, the most common causes for revision were different with rotator cuff tears for total shoulder replacement and glenoid component loosening for Reverse total shoulder replacement.
A September 2023 paper in the Journal of shoulder and elbow surgery (11) suggested that primary (first) revision and (second) anatomic and reverse total shoulder replacement in patients 80 years and older “are safe and effective, demonstrating low rates of perioperative mortality and reoperation, durability that exceeds patient longevity (the replacement outlasted the patient), satisfactory postoperative range of motion, and excellent pain relief.”
The researchers did note late complications ranged from 5.6-24% for anatomic total shoulder replacement patients and 3.5-29% for patients undergoing revision shoulder replacement for all indications. Common complications included glenoid loosening (0-18%) and rotator cuff tear (5.6-10%) following anatomic total shoulder replacement and scapular notching (the replacement is wearing away the scapula) (0-40%) and scapular fracture (4-9.4%) following reverse total shoulder replacement . Reoperation rates ranged from 0-6% following anatomic total shoulder replacement and 0-13% following reverse total shoulder replacement.
A February 2024 study (12) added the consideration of mental health in older patients: “Considering the fact that mental health illnesses increase with age, and that shoulder arthroplasty procedures are often indicated in the older population, exploring the relationship between mental health and shoulder arthroplasty outcomes can have pivotal implications for shoulder surgeons and patients worldwide. The literature has shown that patients with poor mental health report lower patient-reported outcomes, higher peri-operative complications (such as anemia, infection, delirium, and others), lengthier hospital stays, and higher readmission rates than the normal patient.”
You have had a successful surgery but still have severe shoulder pain.
Researchers tried to gauge what constituted the minimum results necessary to call a shoulder replacement surgery a success.

In the Journal of shoulder and elbow surgery, (13) researchers tried to gauge what constituted the minimum results necessary to call a shoulder replacement surgery a success. In 326 patients who had either a total shoulder replacement, a primary reverse shoulder replacement, or hemiarthroplasty, in averaging out the patient response outcomes, the researchers found that patients treated with a shoulder arthroplasty require a 1.4-point improvement in the visual analogue pain score (a scoring system of 0- no pain and 10 extreme pain), most of you reading this article will be very aware of this pain scoring system and how it works).
- If you went to surgery with, for an example 8.4 VAS score or very severe pain, you qualified for a minimal clinically important difference (success) if you reported that pain down to a 7.0. The successful surgery still left you in severe pain. Any pain relief is welcome, but how many people would have the surgery for a 10% improvement?
Why patients fail to achieve the minimal acceptable results
to consider the surgery successful?
A November 2021 study (14) compared patient-reported outcomes (PROs) and range of motion (ROM) measurements between patients achieving and failing to achieve a Patient Acceptable Symptom State (PASS) after anatomic total shoulder arthroplasty (replacement) to determine which patient-reported outcomes (PROs) questions and range of motion (ROM) measurements were the primary drivers of poor outcomes.
In this study 301 patients who had undergone primary total shoulder replacement at least two years prior. The primary outcome was the difference in active range of motion (ROM) between patients achieving and failing to achieve the Patient Acceptable Symptom State (minimum requirement) threshold for the American Shoulder and Elbow Surgeons (ASES) and Single Assessment Numeric Evaluation (SANE) scores. The secondary outcome was the difference in self-reported pain levels between those achieving and failing to achieve the minimum requirement.
- Based on the American Shoulder and Elbow Surgeons Patient Acceptable Symptom State threshold, 87% (261/301) of patients achieved a minimally successful total shoulder replacement, whereas 13% did not.
- Based on the Single Assessment Numeric Evaluation Patient Acceptable Symptom State threshold, 69% (208/301) of patients achieved a achieved a minimally successful total shoulder replacement, whereas 31% did not.
- Patients who failed were younger and had lower short form-12 mental health scores than those who did.
- There was a significant difference in pain between those who achieved and failed to achieve a minimally successful total shoulder replacement.
- Those failing had significantly higher pain levels and worse function.
Conclusion: There is variability in the percentage of patients who achieve a a minimally successful total shoulder replacement, ranging from 69% to 87% depending on the patient-reported outcome scoring systems used to define the threshold. Patients who did not achieve a minimally successful total shoulder replacement were significantly more likely to have pain, whereas there were very few differences in range of motion, indicating pain as the primary driver of failing to achieve a successful surgery.
How strong is your shoulder after shoulder replacement?
“While some patients saw improvement in function, surgeon (and patient) should be aware that durability and strength of rotation would be weak.”
Beyond pain, there is the question of function, strength and durability of the replaced shoulder. There is a lot of research focusing on a patient’s ability to resume normal activity or return to their favorite sport after shoulder replacement. Many studies suggest a great deal of success in the shoulder replacement. Other studies are less favorable.
A study from November 2019 (15) compared the isometric strength and endurance of shoulder abduction and internal and external rotation between operated shoulders and non-operated shoulders in the same patient. The patient underwent reverse shoulder replacement due to degenerative rotator cuff tear.
Who was in this study?
- 41 consecutive patients (average age of about 71 years old; 36 females vs 5 males) who underwent reverse shoulder replacement. All 41 patients had no symptoms in the other shoulder and normal shoulder function.
- The average length of follow-up was 34 months.
Results
- Patients exhibited improvement in functional level in the replacement shoulder.
- The limitations however following surgery were In the strength and endurance of internal and external rotation which were lower in operated shoulders than the patient’s other shoulder. The durability of internal and external rotation were significantly lower in operated shoulders.
- While some patients saw improvement in function, surgeon (and patient) should be aware that durability and strength of rotation would be weak.
“There is currently no consensus on recommended levels of activity and sport following reverse total shoulder arthroplasty.”
From July 2019 and the journal Shoulder & Elbow.(16)
- “Reverse total shoulder arthroplasty is now the most frequently performed form of shoulder replacement. There is currently no consensus on recommended levels of activity and sport following Reverse total shoulder arthroplasty.”
- “Return to sport is tolerated following Reverse total shoulder arthroplasty; however, studies are short to medium term only and although the reported complication rate is low, the studies did not include radiographic evaluation. Longer term studies with subgroup analysis evaluating common recreational activities after Reverse total shoulder arthroplasty are required, particularly in the younger population, in order to establish clear post-operative guidelines.”
In April 2024 (17) this line of research was continued by doctors looking to suggest recommendations for post- surgical rehab. They write: “There is no consensus concerning the rehabilitation protocol following reverse shoulder replacement. Several patients are expecting to be able to use their arms for sports or recreation shortly after their operation.” What they found was: At 3 months post-op, forward flexion was found to be significantly higher in the early rehabilitation group than the the delayed rehabilitation group. Twelve months post-op, no significant difference in any clinical or patient-reported outcome was shown. More complications were reported in the 6 weeks-delayed rehabilitation group. They continue: immediate shoulder mobilization but may not be applied to every patient.”
Poor lifestyle choices and failed shoulder replacement
In a paper published in the March 2017 issue of the Journal of Shoulder and Elbow Surgery, (18) doctors in Germany evaluated and identified risk factors for the development of intraoperative and postoperative surgical complications in total shoulder arthroplasty in patients with primary osteoarthritis. Twenty-seven complications (9.8%) in 275 shoulder arthroplasties were recorded. Mostly from patients who practiced poor lifestyle choices, at the top of the list smoking and alcohol consumption.
A July 2024 (19) study associated alcohol abuse with increased rates of 2-year revision surgery, as well as 90-day readmission and 90-day transient mental disorder following primary shoulder replacement for osteoarthritis.
An October 2023 study (20) suggested that patients who quit smoking at least 1 month before shoulder replacement surgery had improved outcomes compared to current smokers. Current smokers had statistically significant higher pain scores or opioid use. Five studies found increased rates of revision surgery in smokers. Smokers were significantly more likely to have increased rates of surgical, wound, superficial, and deep surgical site complications.
These are just a few of the studies which if you read them as a whole tells us that patients with poor lifestyle choices, those who do not bounce back well from adversity, those whose shoulders have significant degeneration of the soft tissue, should be offered an alternative to shoulder replacement.
A February 2025, (36) study looked at the issues morbidly obese patients who had reverse shoulder replacement. The study matched 4850 morbid obese patients against 55,075 control patients.
- Major complications were more common in the morbidly obese patients including:
- periprosthetic dislocation
- deep vein thrombosis
- blood loss anemia
- and acute renal failure
Mental health issues and failed shoulder replacement
A May 2024 study (21) found: “Patients with mental health conditions may have lower preoperative range of motion, worse postoperative shoulder function, and higher postoperative pain levels than patients without mental health conditions. Patients with mental health conditions demonstrated improvements in range of motion and functional outcomes after shoulder replacement but had higher reported complication and revision rates when compared to patients without mental health conditions . Depression and anxiety were the leading conditions correlated with lower outcomes in patients with mental health conditions after shoulder replacement.”
In a February 2017 issue, doctors at the Steadman Hawkins Clinic of the Carolinas wrote that patients’ resilience, that is the ability to bounce back or recover from stress, an increasingly recognized psychometric property, would do better than patients who do not do well with stress. The patients with low resilience would suffer from greater shoulder complications.(22)
Seven years later in February 2024, this topic is still considered a controversial idea as demonstrated by a more recent study (23): “Patient resilience is inconsistently demonstrated to affect clinical outcomes associated with joint preserving and arthroscopic surgery. However, substantial limitations in the existing literature including underpowered sample sizes, lack of standardization in stratifying patients based on pretreatment resilience, and inconsistent collection of PROs throughout the continuum of care, diminish the strength of most conclusions that have been drawn.
Seven years of past research 2017-2024 on shoulder replacement complications –
where are we today?
In the worst case of shoulder replacement I have seen, an elderly man presented with right shoulder pain. When I asked him to lift his arms, he lifted his right arm, but had no motion at all in his left shoulder. I was perplexed and asked if his left shoulder also hurt. His response was alarming. He told me he had a left shoulder replacement, and the arm prosthesis had dislocated out the the shoulder, and he had absolutely no use of his left arm since the dislocation that could not be relocated into the false joint. He obviously wanted to avoid surgery to his right shoulder.
Again we can go back to 2017 and see problems facing doctors still not resolved in 2024. In 2017 doctors at the University Medical Center of Cologne in Germany also published research (24) in which a bad shoulder problem is can be made much worse by shoulder replacement. The German doctors suggest that a preoperative evaluation of humeral head subluxation (the head of the shoulder is not where it is supposed to be) and glenoid erosion (the shoulder labrum has deteriorated), two factors associated with less favorable postoperative shoulder replacement results, should be considered before moving forward to surgery.
In May 2022 surgeons (25) looked ta the various techniques exist to manage complex primary glenohumeral osteoarthritis with posterior subluxation and posterior glenoid erosion. (The head of the shoulder is not where it is supposed to be the bone has eroded). The recommendation here was reverse shoulder replacement to prevent posterior subluxation, complications and the need for revision surgery.
Here is a report from doctors at the Mayo Clinic. It was published in the Journal of shoulder and elbow surgery (26) December 18, 2017 edition. Here are the highlights:
- 42 patients who had shoulder replacement, two patients had both shoulders replaced. Minimum 10 year follow up. Goal: Long-term assessment of shoulder replacement
- Studies have demonstrated mixed results after humeral head replacement for osteoarthritis at short- and medium-term follow-up intervals.
- Some patients experienced significant pain relief postoperatively that was maintained during the long-term follow-up
- 11 patients more than 25% of the study group reported persistent moderate or severe pain minimum ten years out
- Ten of 44 (22.7%) shoulders underwent revision surgery, predominantly for glenoid arthrosis (arthritis).
- In the 25 shoulders with 5 years of radiographic follow-up, patients demonstrated moderate to severe glenoid erosion in 50% at 5 years, which increased to 59% at 15 years and 88% at 20 years.
“Humeral head replacement remains a successful operation for osteoarthritis at long-term follow-up. However, there is a substantive subgroup with continuing pain and a high rate of glenoid bone erosion after 10 years. Surgeons should carefully consider patients’ needs and desires when judging the indications for humeral head replacement.
In June 2024 (27) doctors evaluated and compared the incidence of complications and revision surgeries between in two of convertible metal-back glenoid systems in total shoulder groups over a follow-up period of up to five years.
- A retrospective analysis included 69 shoulders from 65 patients with primary shoulder replacement and receiving humeral head replacement with a metal component. The patients were divided into two groups. Metal-backed glenoid implants with both stemless and stemmed humeral components
- Clinical and radiological assessments were conducted at 2, 5, and 10 years postoperatively.
- Both implant types showed comparable revision rates and survival probabilities. Rotator cuff insufficiency and polyethylene wear are the two most common complications leading to revision.
- The researchers also noted that complications caused them to change the patient monitoring schedule: “To facilitate ongoing monitoring and optimize patient safety, we implemented a modification in the follow-up protocol, transitioning to annual appointments or earlier when necessary. This study underscores the unsolved disadvantages in metal-back components and the importance of a mid- to long-term longitudinal assessment of those patients.”
Despite research showing increasing numbers of surgical failures, more patients are having shoulder replacement surgery.
The above study shows the concern for the high number of complications measured long-term in shoulder replacement patients. This was a concern in 2016. In a study published in the journal Radiographics, radiologists (28) looked for key imaging features in patient shoulders to help them distinguish between the shoulder problems listed above. If they could find MRI evidence for the source of pain, radiologists could guide surgeons in choosing the type of replacement surgery the patients should get. This they suggested would help limit surgical failures and get the shoulder to as normal a range of motion as possible.
Sounds good, but as we have seen in patients here in our clinic that had an MRI, had the source of their pain pinpointed, had preoperative planning, had the best prosthetic device for them, had the best intention of the health providers to get that shoulder to as good as new as possible. The surgery still failed catastrophically.
In a study in the Journal of Elbow and Shoulder Surgery, doctors put a great degree of surgical failure on the shoulder instability the surgery itself caused.
Here is the researchers report:(29)
- 27 patient case studies were reviewed. These patients had experienced shoulder replacement postoperative instability
- The type of surgeries were 8 hemiarthroplasties (ball replacement and structural fix of the bone),
- 14 total shoulder replacements with metal-backed glenoid components, and
- 5 total shoulder replacements with cemented glenoid components.
The patients had:
- 10 isolated subscapularis tears,
- 6 massive rotator cuff tears,
- 8 component malpositions,
- 2 component dissociations or loosening, and
- 1 humeral shortening.
As pointed out above, stress from surgery can put a lot of pressure on a rotator cuff tendon. This can cause component loosening.
As mentioned above, a problem with shoulder replacement is bone disintegration. From one research study: “Subchondral bone changes associated with osteoarthritis may be important factors to consider when choosing a replacement component. For surgical treatment, many implant options exist, and survivability is often dependent on patient age, activity level, and progression of osteoarthritis.”(30)
A paper from December 2021 (31) examined if the severity of osteoarthritis and the development of bone spurs at the acromioclavicular joint would lead to post reverse shoulder replacement fractures of the acromial and scapular spine fractures. In this study 11 patients, who were about 70 years old, who had complications were matched to 44 patients who did not. The patients who suffered either an acromial or scapular spine fractures post-operatively had worse acromioclavicular joint osteoarthritis larger osteophyte or bone spur formation.
One thing certainly that would help prevent surgical failure is not having a surgery.
In the Mayo clinic study above, bone disintegration was a great concern. In a recent study, also in the Journal of shoulder and elbow surgery, doctors discuss hardware failures known to plague patients: “The longevity of total shoulder replacement is primarily limited by the performance of the ultra high-molecular-weight polyethylene glenoid component. [This study] demonstrates that glenoid component fracture associated with oxidation has not been eliminated with the advent of modern materials (HXL) in the shoulder domain.”
In other words, the hardware caused an oxidation problem which disintegrated the bone.(32)
The health of bone is obviously very important in shoulder replacement. As you can imagine a revision surgery to fix the problems created by bone disintegration caused by the first replacement will be a complex one.
The following research also from the Journal of Shoulder and Elbow Surgery explains why patients must be given information on treatment options outside of surgery:
- “The management of a failed shoulder represents a complex and difficult problem for the treating surgeon, with potential difficulties and complications that are related to the need to remove a well-fixed stem.”(33)
An August 2022 study (34) updated this information by suggesting: “Nowadays, surgeons try to balance the need for a stable fixation of the humeral component with the potential need for revision surgery. Complications of revision shoulder arthroplasty are related to the need for removing a well-fixed humeral stem, the length of the procedure, and the need to treat severe bone loss.”
If the prosthesis is removed due to failure, the bone becomes compromised, and it is even more difficult to place another prosthesis.
A March 2024 study (35) assessed functional outcomes and survivorship following revision shoulder replacement. The authors write: “Revision shoulder arthroplasty is a surgical procedure performed to address complications or failures of primary total shoulder replacement. However, limited evidence exists regarding the functional outcomes and longevity of implants following revision.”
In this study, patients who had revision reverse shoulder replacement following a failed shoulder replacement were studied. The average age of the patient at first surgery was about 60 years old. The average time between the need for the second surgery was 4.5 to 5 years.
- Revision surgery significantly improved functional outcomes in forward elevation, external rotation, internal rotation, and forward elevation strength. Patients also reported very mild pain. The overall 2-, 5-, and 10-year post-revision implant survival rate was 85.48%, 83.06%, and 79.84%, respectively.
Do you need help with your shoulder pain?
Call for a free phone consultation with our staff 800-300-9300
Related articles
What is a normal shoulder MRI and what is an abnormal shoulder MRI?
References
1 Cooper KS, Powell GM, Baffour FI, Johnson MP, Frick MA. Incidence of complications related to shoulder arthroplasties identified on computed tomography. Emergency Radiology. 2023 Aug;30(4):475-83.
2 Ödquist M, Hallberg K, Rahme H, Salomonsson B, Rosso A. Lower age increases the risk of revision for stemmed and resurfacing shoulder hemi arthroplasty: A study from the Swedish shoulder arthroplasty register. Acta orthopaedica. 2017 Dec 5:1-7.
3 Nolte PC, Elrick BP, Arner JW, Ridley TJ, Woolson TE, Tross AK, Midtgaard KS, Millett PJ. Total Shoulder Arthroplasty After Previous Arthroscopic Surgery for Glenohumeral Osteoarthritis: A Case-Control Matched Cohort Study. The American Journal of Sports Medicine. 2021 Jun;49(7):1839-46.
4 Liu H, Huang TC, Yu H, Wang Y, Wang D, Long Z. Total shoulder arthroplasty versus reverse total shoulder arthroplasty: Outcome comparison in osteoarthritis patients with or without concurrent rotator cuff deficiency. Medicine (Baltimore). 2022 Aug 12;101(32):e29896.
5 Reddy C, Venishetty N, Jones H, Mounasamy V, Sambandam S. Factors that increase the rate of periprosthetic dislocation after reverse shoulder arthroplasty. Arthroplasty. 2023 Dec 2;5(1):57.
6 Sinkler MA, Dolan JD, Henderson D, Steflik MJ, Lewis FD, Parada SA, Crosby LA. Risk factors of instability following reverse total shoulder arthroplasty in patients with no history of shoulder surgery. Journal of Orthopaedics. 2022 Nov 1;34:339-43.
7 Townsend CB, Wright J, Wright TW, Pazik M, Schoch B, Gil J, King JJ. Severe acromioclavicular joint osteoarthritis is associated with acromial stress fractures after reverse shoulder arthroplasty. JSES international. 2022 Mar 1;6(2):236-40.
8 Rasmussen JV, Olsen BS. Previous surgery for instability is a risk factor for a worse patient-reported outcome after anatomical shoulder arthroplasty for osteoarthritis: a Danish nationwide cohort study of 3,743 arthroplasties. Acta Orthopaedica. 2022;93:588.
9 Ravi V, Murphy RJ, Moverley R, Derias M, Phadnis J. Outcome and complications following revision shoulder arthroplasty: a systematic review and meta-analysis. Bone & Joint Open. 2021 Aug 2;2(8):618-30.
10 Orvets ND, Chan PH, Taylor JM, Prentice HA, Navarro RA, Garcia IA. Similar rates of revision surgery following primary anatomic compared to reverse shoulder arthroplasty in patients≥ 70 years old with glenohumeral osteoarthritis: A cohort study of 3,791 patients. Journal of Shoulder and Elbow Surgery. 2023 Apr 17.
11 DeBernardis DA, Zhang T, Duong A, Fleckenstein CM, Almasri M, Hasan SS. Total Shoulder Arthroplasty in Patients Aged 80 Years and Older: A Systematic Review. J Shoulder Elbow Surg. 2023 Sep 9:S1058-2746(23)00649-3.
12 Daher M, Boufadel P, Lopez R, Chalhoub R, Fares MY, Abboud JA. Beyond the joint: Exploring the interplay between mental health and shoulder arthroplasty outcomes. Journal of Orthopaedics. 2024 Feb 10.
13 Tashjian RZ, Hung M, Keener JD, Bowen RC, McAllister J, Chen W, Ebersole G, Granger EK, Chamberlain AM. Determining the minimal clinically important difference for the American Shoulder and Elbow Surgeons score, Simple Shoulder Test, and visual analog scale (VAS) measuring pain after shoulder arthroplasty. Journal of shoulder and elbow surgery. 2017 Jan 1;26(1):144-8.
14 Cole EW, Moulton SG, Werner BC, Denard PJ. Why patients fail to achieve a Patient Acceptable Symptom State (PASS) after total shoulder arthroplasty?. JSES international. 2022 Jan 1;6(1):49-55.
15 Erşen A, Birişik F, Bayram S, Şahinkaya T, Demirel M, Atalar AC, Demirhan M. Isokinetic Evaluation of Shoulder Strength and Endurance after Reverse Shoulder Arthroplasty: A Comparative Study. Acta Orthop Traumatol Turc. 2019 Nov;53(6):452-456. doi: 10.1016/j.aott.2019.08.001. Epub 2019 Aug 19. PMID: 31439480; PMCID: PMC6939012.
16 MacInnes SJ, Mackie KE, Titchener A, Gibbons R, Wang AW. Activity following reverse total shoulder arthroplasty: What should surgeons be advising?. Shoulder & elbow. 2019 Jul;11(2_suppl):4-15.
17 Sachinis NP, Yiannakopoulos CK, Berthold DP, Franz A, Beitzel K. Can we accelerate rehabilitation following reverse shoulder arthroplasty? A systematic review. Shoulder & Elbow. 2024 Apr;16(2):214-27.
18 Leschinger T, Raiss P, Loew M, Zeifang F. Predictors of medium-term clinical outcomes after total shoulder arthroplasty. Arch Orthop Trauma Surg. 2017 Feb;137(2):187-193. doi: 10.1007/s00402-016-2602-x. Epub 2016 Dec 7.
19 Chiu AK, Cuero KJ, Agarwal AR, Fuller SI, Kreulen RT, Best MJ, Srikumaran U. The association of alcohol use disorder with revision rates and post-operative complications in total shoulder arthroplasty. Shoulder & Elbow. 2024 Jul;16(3):250-7.
20 Kamma SA, Pathapati RK, Somerson JS. Smoking cessation prior to total shoulder arthroplasty: a systematic review of outcomes and complications. Shoulder & Elbow. 2023 Oct;15(5):484-96.
21 Jochl OM, Afeste EK, Garg S, Kanakamedala AC, Lind DR, Hinz M, Rizzo M, Millett PJ, Ruzbarsky J, Provencher MT. The Impact of Mental Health Conditions on Clinical and Functional Outcomes after Shoulder Arthroplasty: A Systematic Review. JSES Reviews, Reports, and Techniques. 2024 May 15.
22 Tokish JM, Kissenberth MJ, Tolan SJ2, et al. Resilience correlates with outcomes after total shoulder arthroplasty. J Shoulder Elbow Surg. 2017 Feb 10. pii: S1058-2746(17)30012-5. doi: 10.1016/j.jse.2016.12.070.
23 DeFoor MT, Cognetti DJ, Bedi A, Carmack Jr DB, Arner JW, DeFroda S, Ernat JJ, Frangiamore SJ, Nuelle CW, Sheean AJ. Patient Resilience Does Not Conclusively Affect Clinical Outcomes Associated With Arthroscopic Surgery but Substantial Limitations of the Literature Exist. Arthroscopy, Sports Medicine, and Rehabilitation. 2024 Apr 1;6(2):100812.
24 Leschinger T, Raiss P, Loew M, Zeifang F. Total shoulder arthroplasty: risk factors for intraoperative and postoperative complications in patients with primary arthritis. J Shoulder Elbow Surg. 2017 Mar;26(3):e71-e77. doi: 10.1016/j.jse.2016.08.001. Epub 2016 Oct 10.
25 Scarcella MJ, Yalcin S, Ginesin E, Patel R, Miniaci A. Treatment options for complex shoulder osteoarthritis with posterior humeral head subluxation and glenoid bone loss (Walch B): A systematic review. JSES Reviews, Reports, and Techniques. 2022 Aug 1;2(3):285-96.
26 Robinson WA, Wagner ER, Cofield R, Sanchez-Sotelo J, Sperling JW. Long-term outcomes of humeral head replacement for the treatment of osteoarthritis; a report of 44 arthroplasties with minimum 10-year follow-up. Journal of shoulder and elbow surgery. 2017 Dec 18.
27 Kraus M, Illner J, Warnhoff M, Brunner M, Schneller T, Lazaridou A, Scheibel M. Complications and Revisions in Metal-Backed Anatomic Total Shoulder Arthroplasty: A Comparative Study of Revision Rates Between Stemless and Stemmed Humeral Components. Journal of Shoulder and Elbow Surgery. 2024 Jun 27.
28 Lin DJ, Wong TT, Kazam JK. Shoulder Arthroplasty, from indications to complications: what the radiologist needs to know. Radiographics. 2016 Jan-Feb;36(1):192-208. doi: 10.1148/rg.2016150055.
29 Kany J, Jose J, Katz D, Werthel JD, Sekaran P, Amaravathi RS, Valenti P. The main cause of instability after unconstrained shoulder prosthesis is soft tissue deficiency. Journal of Shoulder and Elbow Surgery. 2017 Feb 27.
30 Knowles NK, Ferreira LM, Athwal GS. The arthritic glenoid: anatomy and arthroplasty designs. Curr Rev Musculoskelet Med. 2016 Jan 23.
31 Townsend CB, Wright J, Wright TW, Pazik M, Schoch B, Gil J, King JJ. Severe acromioclavicular joint osteoarthritis is associated with acromial stress fractures after reverse shoulder arthroplasty. JSES international. 2022 Mar 1;6(2):236-40.
32 Ansari F, Lee T, Malito L, Martin A, Gunther SB, Harmsen S, Norris TR, Ries M, Van Citters D, Pruitt L. Analysis of severely fractured glenoid components: clinical consequences of biomechanics, design, and materials selection on implant performance. J Shoulder Elbow Surg. 2016 Jan 14. pii: S1058-2746(15)00588-1. doi: 10.1016/j.jse.2015.10.017
33 Cisneros LG, Atoun E, Abraham R, Tsvieli O, Bruguera J, Levy O. Revision shoulder arthroplasty: does the stem really matter?. Journal of shoulder and elbow surgery. 2016 May 1;25(5):747-55.
34 Buch B, Vall M, Consigliere P, Guillén JA, Cruz E, Natera L. Short stems and stemless shoulder arthroplasty: current concepts review. Archives of Bone and Joint Surgery. 2022 Aug;10(8):633.
35 Katayama ES, Barry LW, Barnett JS, Iyer AI, Patel AV, Bishop JY, Cvetanovich GL, Rauck RC. Functional outcomes and survivorship following aseptic revision shoulder arthroplasty. Journal of Orthopaedics. 2024 Aug 1;54:51-6.
36 Areti A, Montanez B, Perake V, Sambandam SN. Impact of morbid obesity on postoperative outcomes in reverse total shoulder arthroplasty: A national inpatient sample analysis. Journal of Orthopaedics. 2025 Oct 1;68:84-9.