Marc Darrow, MD, JD.
A doctor will diagnose failed sacroiliac (SI) joint fusion surgery after the patient continues to suffer from chronic pain and loss of function after the their procedure. There are many reasons why the surgery has failed. This includes pseudarthrosis (a non-union of the bones), The implants has loosened or caused fracture of the bone. Or a new onset of pain has developed. This new pain can be caused by altered mechanics and gait.
Failed sacroiliac joint fusion surgery affects a little less than 3% of patients undergoing sacroiliac joint fusion surgery. In a January 2024 study (1) doctors wrote of their analysis of patient outcome data in this group of failed surgery patients.
“(This) study demonstrates patients undergoing revision surgery have moderate improvement in low back pain, however, few have complete resolution of their symptoms. Specific patient factors, such as chronic opiate use and female sex may decrease the expected improvement in patient-reported outcomes following surgery. Failure to obtain relief may be due to incorrect indications, lack of biologic fusion and/or presence of co-pathologies.”
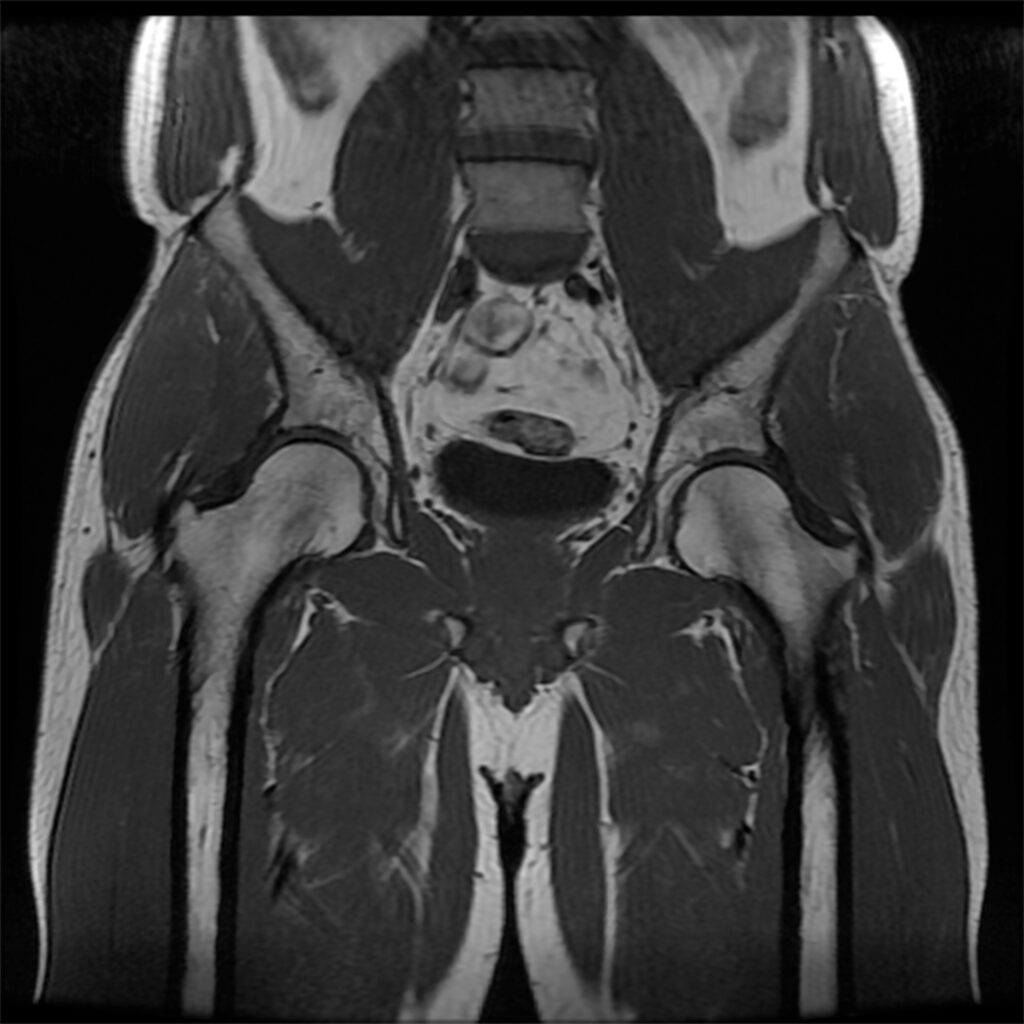
An August 2024 study(2) examined sacroiliac joint degeneration after lumbar or lumbosacral fusion surgery. In this study, researchers investigated whether multi-segment fusion or fusion-to-sacrum increases the risk of sacroiliac joint pathology, compared with single-segment fusion or a non-fused sacrum.
- This study included 116 patients who underwent lumbar or lumbosacral fusion and were followed up for 2 years.
- The patients were classified into single-segment fusion (46 patients) and multi-segment fusion (more than two-levels, 70 patients) groups and then reclassified into the non-fused sacrum (68 patients) and fusion-to-sacrum groups (48 patients). Low back pain was assessed using a visual analog scale (VAS, 0 none – 10 unbearable pain).
Low back pain VAS scores significantly differed at 6 months (single-segment fusion, 3 on a scale of 10 (mild pain) to multi-segment fusion, 4.8 on a scale of 10, moderate approaching severe pain) and 2 years postoperatively (still mild pain), (still moderate approaching severe pain).
There was no significant difference in sacroiliac joint degeneration, as assessed by CT scan, between the two surgical groups: 14 (30%) and 19 (27%) patients in the single-segment and multi-segment fusion groups, respectively. Somewhat similar findings in non-fused sacrum compared to fusion-to-sacrum patients showed mild pain at one year and at two years, non-fused sacrum, mild pain, but, fusion-to-sacrum patients showed moderate approaching severe pain. CT scan revealed that 18 (26%) and 15 (31%) patients in the non-fused sacrum and fusion-to-sacrum groups, respectively.
Neurosurgeons suggest that treatment for sacroiliac joint pain should not include spinal fusion.
This is the title of a paper published in the journal Neurosurgery clinics of North America : “Sacroiliac Fusion: Another “Magic Bullet” Destined for Disrepute.”(3)
This is what the paper says:
“Pain related to joint dysfunction can be treated with joint fusion; this is a long-standing principle of musculoskeletal surgery. However, pain arising from the sacroiliac joint is difficult to diagnose. . . Evidence establishing (successful) outcomes (of spinal fusion) is misleading because of vague diagnostic criteria, flawed methodology, bias, and limited follow-up. Because of non-standardized indications and historically inferior reconstruction techniques, SI joint fusion should be considered unproven. The indications and procedure in their present form are unlikely to stand up to close scrutiny or weather the test of time.”
There are many people who may disagree that fusion will not help sacroiliac joint pain. Many people do in fact do get pain relief and benefit from surgery. I don’t see this people in my office. I see the people who did not do well after surgery. A December 2019 still asked “What do we know about the biomechanics of the sacroiliac joint and of sacropelvic fixation?” (4)
Here is an explanation of why this surgery may work for some, but may not work for others. “The sacroiliac joint is characterized by a large variability of shape and ranges of motion among individuals. Although the ligament network and the anatomical features strongly limit the joint movements, sacroiliac displacements and rotations are not negligible.
Currently available treatments for sacroiliac joint dysfunction include physical therapy, steroid injections, Radio-frequency ablation of specific neural structures, and open or minimally invasive SIJ fusion. Several studies reported the clinical outcomes of the different techniques and investigated the biomechanical stability of the relative construct (the construct being the fusion itself), but the effect of sacropelvic fixation techniques on the joint flexibility and on the stress generated into the bone is still unknown. In our opinion, more biomechanical analyses on the behavior of the sacroiliac joint may be performed in order to better predict the risk of failure or instability of the joint.”
“The sacroiliac joint has been estimated to contribute to pain in as much as 38% of cases of lower back pain. There are no clear diagnostic or treatment pathways. . . “
This is a study from December 2020. The doctors in this study use a much stronger language to describe the overreliance of SIJ Fusion. The paper was published in the Journal of pain research. (5)
“The sacroiliac joint has been estimated to contribute to pain in as much as 38% of cases of lower back pain. There are no clear diagnostic or treatment pathways. . . “
Here are some of the points provided by this study:
- “Proposed criteria for diagnosis of sacroiliac joint dysfunction can include pain in the area of the sacroiliac joint, reproducible pain with provocative maneuvers, and pain relief with a local anesthetic injection into the SIJ.
- Conventional non-surgical therapies such as medications, physical therapy, radiofrequency denervation, and direct SI joint injections may have some limited durability in therapeutic benefit. Surgical fixation can be by a lateral or posterior/posterior oblique approach with the literature supporting minimally invasive options for improving pain and function and maintaining a low adverse event profile.
- SIJ pain is felt to be an underdiagnosed and undertreated element of low back pain. There is an emerging disconnect between the growing incidence of diagnosed SI pathology and underwhelming treatment efficacy of medical treatment. This has led to an increase in SI joint fixation (fusions).”
SI Fusion is probably better than traditional conservative care treatments
An August 2022 study (6) found that: “Among patients meeting diagnostic criteria for SI joint pain and who have not responded to conservative care, minimally invasive SI joint fusion is probably more effective than conservative management for reducing pain and opioid use and improving physical function and Quality of Life.” Also noted from these researchers is that side effects and complications “appear to be higher for minimally invasive SI joint fusion than conservative management through 6 months. Based on evidence from uncontrolled studies, serious adverse effects from minimally invasive SI joint fusion may be higher in usual practice compared to what is reported in trials.”
Post-operative opioid use
In December 2023 researchers (7) evaluated the duration and magnitude of post-operative opioid prescriptions after minimally invasive surgical sacroiliac joint fusion as compared to other common spine surgeries. The researchers acknowledge that minimally invasive surgical sacroiliac joint fusion “has been reported to significantly improve quality of life and reduce pain. However, there is a (lack) of reported data on post-operative opioid use in patients undergoing minimally invasive surgical sacroiliac joint fusion for sacroiliac joint dysfunction. In a survey of 4,666 patients who underwent minimally invasive surgical sacroiliac joint fusion, the researchers found patients “continued to fill opioid prescriptions 1-year post-operatively at significantly higher proportions than those undergoing other common spine procedures . . . pre-surgery chronic opioid users filled the highest opiate dosages during the 30-day post-operative period. The conclusion of this research was “minimally invasive surgical sacroiliac joint fusion may result in less effective pain reduction when compared to other common spine surgeries. . . ”
Contact us and related articles
If you have chronic back pain, have had painkillers, physical therapy, and other conservative care options that have not helped, and, now you are being told to have another surgery, we may be able to help reduce pain and increase function non-surgically. Regenerative medicine injections may be an alternative for you. Many people benefit from these treatments, but, they do not work for everyone. Will it work for you? Get a FREE phone consultation.
Call for a free phone consultation with our staff 800-300-9300
Related articles
Failed Back Surgery Syndrome: Conservative care, Spinal Cord Stimulators
Misdiagnosis – When it may not be Sacroiliac joint dysfunction
Are MRIs sending people to back surgery who may not need back surgery?
References
1 Brown L, Swiontkowski M, Odland K, Polly DW, Haselhuhn J. Effect of revision sacroiliac joint fusion on unresolved pain and disability: a retrospective cohort study. European Spine Journal. 2024 Jan 9:1-0.
2 Shin JW, Suk YJ, Park Y, Ha JW, Kim HS, Suk KS, Moon SH, Park SY, Lee BH, Kwon JW. Sacroiliac joint degeneration after lumbar or lumbosacral fusion surgery-a comparative study of the number of fused segments and sacral fusion. World neurosurgery.:S1878-8750
3 Bina RW, Hurlbert RJ. Sacroiliac Fusion: Another “Magic Bullet” Destined for Disrepute. Neurosurgery Clinics of North America. 2017 Jul 31;28(3):313-20.
4 Casaroli G, Bassani T, Brayda-Bruno M, Luca A, Galbusera F. What do we know about the biomechanics of the sacroiliac joint and of sacropelvic fixation? A literature review. Medical Engineering & Physics. 2019 Dec 19.
5 Falowski S, Sayed D, Pope J, Patterson D, Fishman M, Gupta M, Mehta P. A Review and Algorithm in the Diagnosis and Treatment of Sacroiliac Joint Pain. Journal of Pain Research. 2020;13:3337.
6 Chang E, Rains C, Ali R, Wines RC, Kahwati LC. Minimally invasive sacroiliac joint fusion for chronic sacroiliac joint pain: a systematic review. The Spine Journal. 2022 Jan 10.
7 Benson D, Litvak A, Zhang D, Johnson C, El Dafrawy M, Lee M. Duration and Magnitude of Opioid Use After Minimally Invasive Sacroiliac Joint Fusion. Spine.:10-97.






