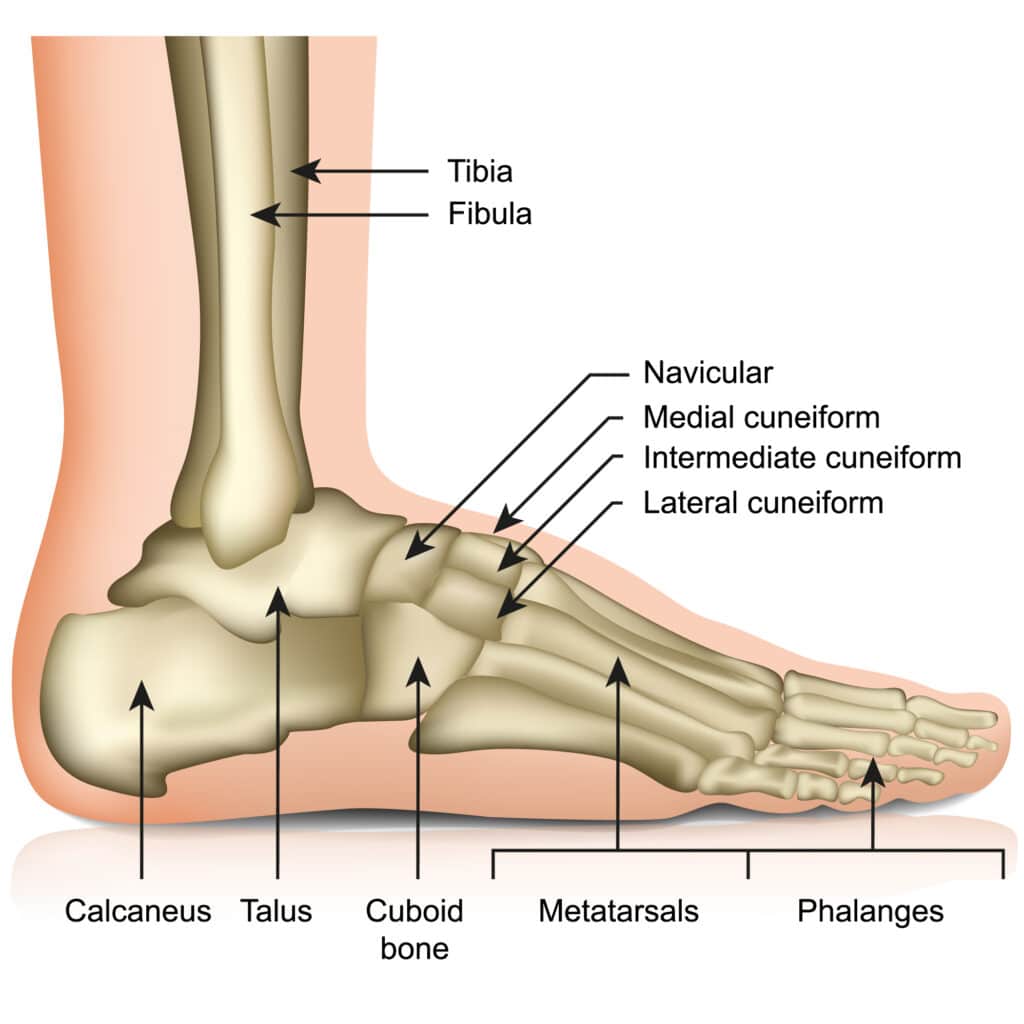
A diagnosis of lesser metatarsophalangeal (the joints at the base of the toe) joint instability means the joints where the toes and the metatarsal bones meet in the forefoot are loose and unstable because of injury or weakness of the ligaments and plantar plate. If left untreated, toe deformity and dislocation of the proximal phalanx (the first bone of the toe) will likely occur.
A December 2024 paper (1) gives a bleak outlook when it comes to certain conservative care treatments: “Conservative treatment options, including the use of nonsteroidal anti-inflammatory medications, intra-articular steroid injections, orthosis, and accommodative shoe modifications, generally provide only temporary relief and do not effectively halt the progression of deformity in most cases.”
Metatarsophalangeal (MTP) instability
A December 2024 paper (2) addresses Metatarsophalangeal (MTP) instability. The authors write that Metatarsophalangeal (MTP) instability is a common cause of metatarsalgia of the lesser toes (the toes not including the big toe). Instability often presents as pain in the plantar forefoot, progressing to coronal (front to back) and transverse plane (horizontal) malalignment. MTP joint dislocation can develop in some cases. The plantar plate plays an integral role in MTP joint stabilization, and injury to the plantar plate is the main contributor to the instability noted at the MTP joint.
Medially wedged foot orthoses with a metatarsal pad
A May 2025 study (3) wrote: “Foot orthoses are commonly prescribed to reduce pain and improve function in individuals with chronic metatarsalgia. Reducing the mechanical overload under the metatarsal heads during locomotion is the central point of the treatment for chronic metatarsalgia.” In this study of 23 individuals (17 females and 6 males), the researchers suggested medially wedged foot orthoses with a metatarsal pad could further reduce pressure loading under the metatarsal heads and modify foot and ankle biomechanics compared to standard foot orthoses.
A June 2022 study (4) assessed risk factors for the need for secondary or revision surgery following metatarsophalangeal (MTP) joint arthroplasty.
In this study, the researchers write: “Revision or conversion to arthrodesis following metatarsophalangeal (MTP) joint arthroplasty are salvage procedures to manage complications of MTP joint arthroplasty. The purpose of this study was to evaluate demographic trends and evaluate influence of patient-related risk factors in those undergoing MTP arthroplasty (joint replacement) revision to arthrodesis (joint fusion).
- Results: 2750 patients underwent primary MTP arthroplasty for diagnosis of hallux rigidus. Of these, 44 (1.6%) underwent revision arthroplasty and 188 patients (6.8%) were revised to arthrodesis within the first 2 years after the first procedure. Multivariate regression analysis indicates that obesity, depression, and steroid use were associated with a statistically significant increase in revision to arthrodesis from primary arthroplasty.
A January 2024 study (5) compared two popular surgical techniques for primary metatarsalgia and the severe instability of lesser metatarsophalangeal joints. One hundred thirteen patients (117 feet) were enrolled in the study.
First surgery: Triple Weil osteotomy (bones are reshaped and refitted) combined with direct plantar plate repair (a fixing / fusion of the plantar plate). This surgery group achieved “good results, including complete pain reduction, elimination of hyperkeratosis, and American Orthopedic Foot and Ankle Society Score improvement, were achieved in 84.7% of the cases.”
Second surgery: Triple Weil osteotomy performed with proximal interphalangeal joint arthrodesis (fusion). This group “demonstrated good results in 52.4% of the cases. ”
A January 2024 study (6) assessed surgical treatment of fifteen patients (17 feet; average age, 66.9 years; average follow-up, 59.4 months; and minimum follow-up, 24 months) with symptomatic hallux valgus accompanied by painful osteoarthritis of the lesser tarsometatarsal joint. In these patients “preoperative midtarsal pain disappeared in 14 feet and decreased in one foot postoperatively. Preoperative metatarsalgia was found in five feet, of which, it disappeared in two feet, decreased in two feet, and transferred to another region in one foot at the latest follow-up. . . Recurrence of hallux valgus (hallux valgus angle ≥20°) was observed in two feet (11.8%). Nonunion of the third tarsometatarsal joint was observed in one foot (3.1% among 32 joints).” The study concludes: “The clinical and radiographic results indicated that operative treatment for hallux valgus with painful osteoarthritis of the lesser tarsometatarsal joint significantly improves forefoot and midfoot pain and function and has low complication rates.”
References
1 Li CC, Lui TH. Lesser Metatarsophalangeal Joint Instability: Arthroscopic Treatment Alternatives. Foot and Ankle Clinics. 2024 Dec 1;29(4):727-39.
2 Ayoola AS, Jastifer JR. Metatarsophalangeal Joint Instability: Anatomy and Physiopathology. Foot and ankle clinics. 2024 Dec 1;29(4):681-90.
3 Payen E, Acien M, Isabelle PL, Turcot K, Begon M, Abboud J, Moisan G. Impact of different foot orthoses on gait biomechanics in individuals with chronic metatarsalgia. Gait & Posture. 2025 Jan 21.
4 Althoff AD, Ramamurti P, Vennitti C, Kamalapathy P, Park JS, Werner BC, Cooper MT. Preoperative Risk Factors for Primary Metatarsophalangeal Arthroplasty Revision to MTP Arthrodesis for Hallux Rigidus. Foot & Ankle International. 2022 Jun 1:10711007221094837.
5 Bobrov DS, Rigin NV, Lychagin AV, Artemov KD, Slinjakov LJ, Kachesov AV. Surgical Treatment of Metatarsalgia and Severe Instability of Lesser Metatarsophalangeal Joints. The Journal of Foot and Ankle Surgery. 2023 Sep 14.
6 Shima H, Togei K, Hirai Y, Yasuda T, Okuda R, Neo M. Operative outcomes of hallux valgus with painful osteoarthritis of the lesser tarsometatarsal joints. Journal of Orthopaedic Science. 2022 Dec 21.






